Medical billing software for optimizing practice revenue.
Medical billing software, along with scheduling and financial reporting software, makes managing your practice easier than ever.
Medical billing software, along with scheduling and financial reporting software, makes managing your practice easier than ever.
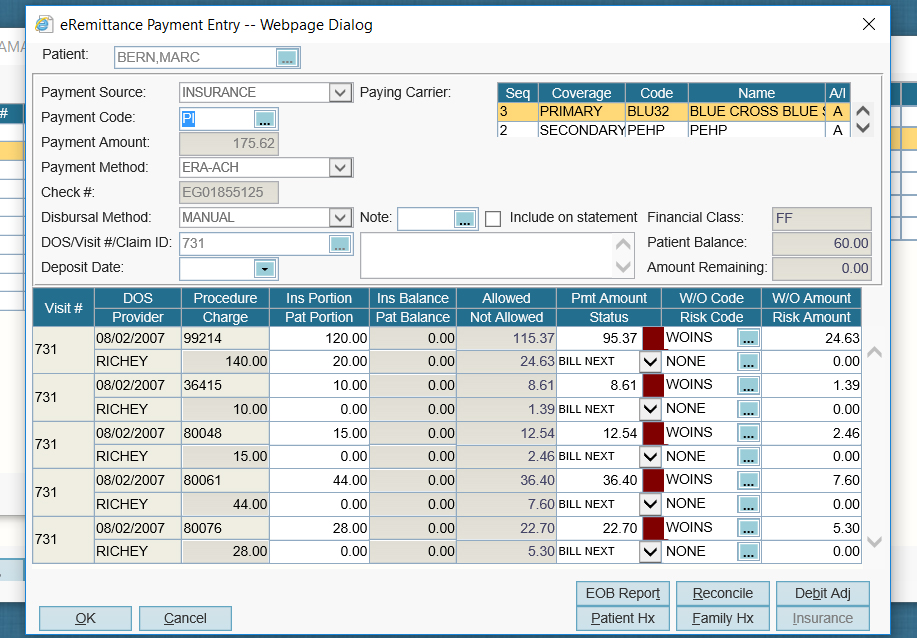
A centralized platform that helps you manage the entire claims process in one location, from charge capture to full reimbursement.
No more uploading claims and downloading remittances. Save time and hassle with our integrated clearinghouse.
Online patient payment solutions to transform your uncollected patient payments and help your practice reduce days in A/R.
All the tools you need to make billing, scheduling, collections, and managing your practice more convenient, intuitive, and productive.
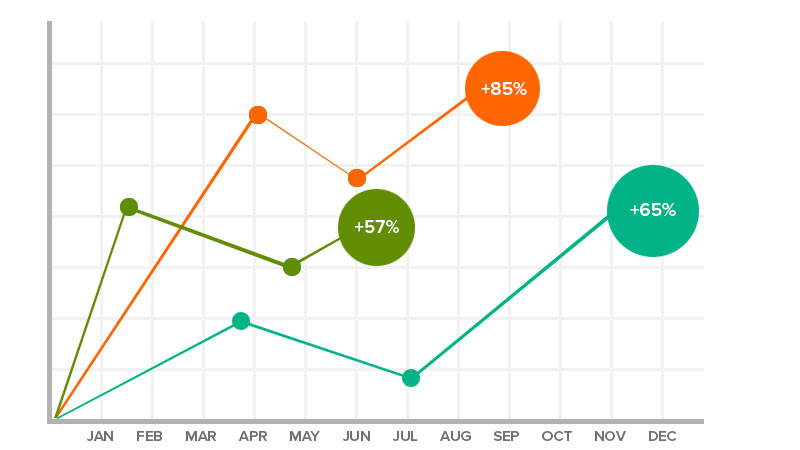
Measure your success and maximize revenue with our exclusive, easy-to-use reporting and business intelligence tools.
Drive revenue with ease. Collections worklists and denial tracking tools take the hassle out of managing receivables so you can collect more, faster.
Our coding software offers a comprehensive suite of tools to make medical coding simple and intuitive for solo to large group practices.
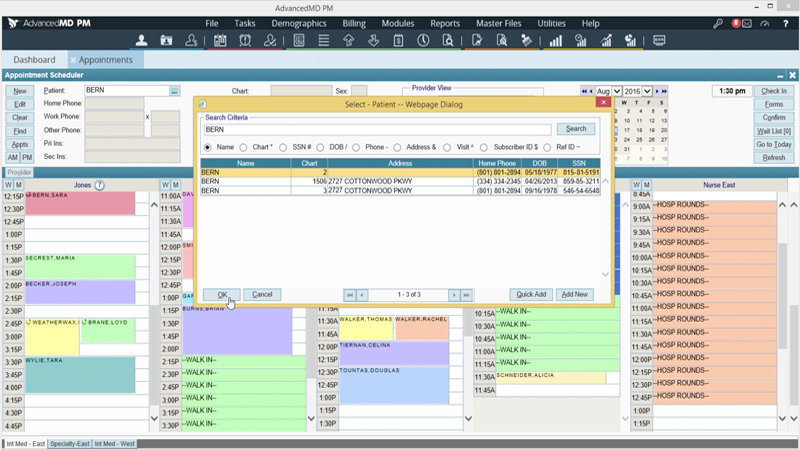
Our billing software is integrated with our scheduling and front office tools so you can collect payments with one-click display of patient information, copays and eligibility.
Billing software that integrates with our credit card processing so you can auto-post charges with just a swipe. Just review and click to confirm – it’s that easy.
Centralized medical billing with powerhouse performance. You can manage billing for each provider and location within a single database and login.
More freedom, less equipment. Cloud-hosted medical billing keeps your data secure & saves you a bundle on equipment and IT costs.
ClaimInspector automatically scrubs your claims for CCI, HIPAA and LCD errors so you see an almost-100% first-pass claim acceptance rate.
Let our data experts handle the data migration from your previous system.
Batch check patient insurance eligibility before appointments or perform on-demand checks with a simple click.
The automated ERA (electronic remittance advice) processing solution for independent practices.
Claims data and copay charges automatically pass into your electronic health records, so you don’t have to worry about manual processes and double data entry.
AdvancedMD, one of the world’s leading medical billing software companies, gives you all the tools you need to manage your claims process in one place and to ensure that your claims management and patient billing process run smoothly every time. Our robust clearinghouse automates manual processes and improves workflow with auto-generated worklists and claims status tracking for multiple providers and sites.
Ensure your schedule stays full so your practice can accommodate more patients. Our powerful scheduling tools let you proactively manage no-shows, cancellations, waitlists and overbooking to maximize your clinical efficiency. Create recurring appointments and reminders to keep your patients and your practice on track.
Make informed financial decisions based on accurate, real-time data and gain a 360-degree view of your practice’s financial health. Our easy-to-read dashboard of interactive tools displays daily updates with MTD, YTD and period comparisons. Take advantage of big data technology, analytics and business intelligence to uncover your hidden revenue opportunities.
Unable to find an answer you’re looking for? No problem. Chat with a live person and we’ll work to get your question answered.
Medical billing software is a computer application that automates the healthcare billing process. Medical practices and billing companies can use this software to greatly improve their reimbursement rates, optimize revenue, and sustain the financial health of their businesses.
Billing software includes functionality to address every part of the medical billing workflow, from scheduling appointments to processing payments. For instance:
Billing software significantly streamlines practice operations in a number of ways. For example:
Prices for our billing software depend on a few factors. We offer both per-provider and per-encounter plans. If your medical practice has a high patient volume, it usually makes sense to opt for a per-provider plan. Practices that see a lower number of patients, and specialties like mental health, chiropractic, and physical therapy, often benefit more from a per-encounter plan.
Prices also depend on added features, such as credit card processing, patient appointment reminders, advanced reporting functionality, and data conversion services.
For more information, visit our pricing page. Feel free to reach out to us – we’d love to help you find the lowest price possible for a plan that meets the needs of your business.
Cloud-based or web-based billing software runs on a remote server and is accessible from any authorized computer that has an internet connection.
When healthcare professionals first started billing electronically, most software systems ran on computers that were physically located in their offices. While this approach was an improvement over submitting claims manually, it came with some drawbacks. Server maintenance, performing ongoing updates, and resolving issues meant medical practices had to invest in trained IT professionals to keep the software running. As technology improved over time, it became possible to run software applications on a remote server and provide access to users through a web browser. This eliminated the need for on-premise software applications.
With cloud- or web-based billing software, maintenance and upgrades are handled entirely by the medical billing software company, and healthcare professionals are able to focus their time on submitting clean claims and getting paid. And as mobile computing becomes more and more a part of everyday life, cloud-based solutions make it easy to perform billing workflows on different types of devices like phones and tablets.
In many cases, medical practices can benefit from having a biller or billing team on-site. Close coordination with providers and quick communication can help streamline the billing workflow and resolve issues as they happen. Over time, a biller’s knowledge of the practice’s revenue cycle can become a powerful asset in optimizing revenue and keeping the business profitable.
That said, outsourcing medical billing is a great option for some practices, especially those without resources to devote to managing the revenue cycle.
Jed Shay, MD
The Pain Care Center
Keith Berkowitz, MD
Center for Balanced Health

Estaban Lavato, MD
La Loma Medical Center
Raju Raval, MD
Read the story ›