Claims management with medical claims software.
Manage each claim from start to finish with a single medical billing claims management platform.
Manage each claim from start to finish with a single medical billing claims management platform.
Ditch the dated, manual processes in favor of tools that automate the work.
ClaimInspector automatically scrubs your claims for CCI, HIPAA & LCD errors so you see an almost-100% first-pass claim acceptance rate.
Fast-track your reimbursements. Web-based claims processing & automatic payment posting help you submit claims & post payments at lightning speed.
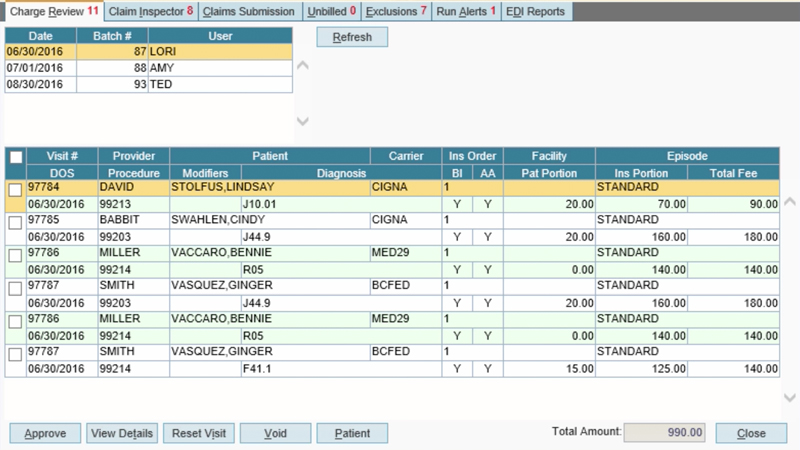
Check charges & make edits directly in the review screen. Build actionable worklists to manage denials, errors or rejections without a hassle.
You do enough. Automate the hassles to substantially increase your profit margin without increasing your workload.
Our medical billing claims management tools are designed to help you save time and receive more revenue. Manual billing processes are replaced by features that automatically scrub, track, review and submit claims for you. Mistakes are caught long before the denials stage so your claims can be submitted quickly and accurately. You’ll get more reimbursements and more revenue with less work.
Our claims management features are part of the AdvancedMD billing software designed to maximize your profitability. AdvancedMD also includes an A/R control center, centralized billing, built-in payment processing features and more.
Rev up your success even more with the AdvancedMD cloud suite, which integrates our billing software with our industry-leading clinical and patient experience systems. This powerhouse medical software platform lets you run your entire practice on a single database, with a single login. It’s the vehicle for a more successful practice.

Change HealthCare has partnered with AdvancedMD to automate and simplify your Claim Attachments process within a unified workflow. We’ve eliminated manual uploading of claims to carrier websites. Emailing and time-consuming manual processes have also been eliminated.
The Change HealthCare application programming interface (API) lets your staff send documents such as clinical notes, images, labs, and EOBs with a claim to carriers – all natively within a natural AdvancedMD workflow to reduce time and effort.
Advantages for Claim Attachments
Enhanced Capabilities

Complete the form below to sign up for a live demo of all AdvancedMD features.