Medical billing software for optimizing practice revenue
Medical billing software, along with scheduling and financial reporting software, makes managing your practice easier than ever.

Claims Management
A centralized platform that helps you manage the entire claims process in one location, from charge capture to full reimbursement.
Clearinghouse
No more uploading claims and downloading remittances. Save time and hassle with our integrated clearinghouse.
Patient Payments
Online patient payment solutions to transform your uncollected patient payments and help your practice reduce days in A/R.
Explore our medical billing software features & add-ons.
All the tools you need to make billing, scheduling, collections, and managing your practice more convenient, intuitive, and productive.
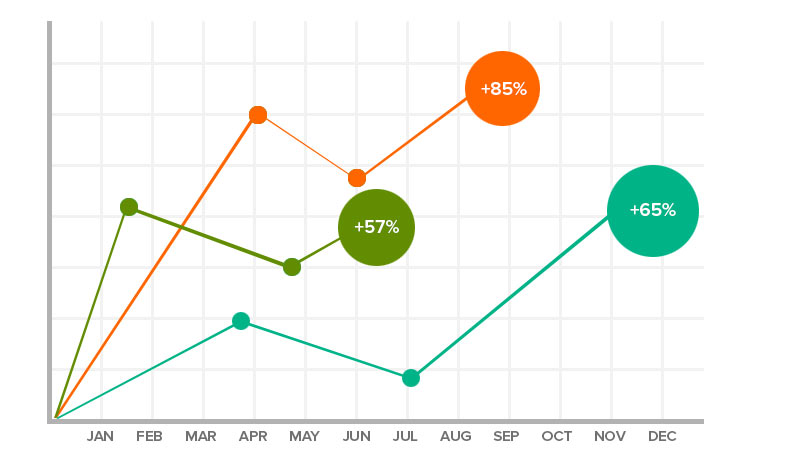
Analytics & Reporting
Measure your success and maximize revenue with our exclusive, easy-to-use reporting and business intelligence tools.
A/R control center
Drive revenue with ease. Collections worklists and denial tracking tools take the hassle out of managing receivables so you can collect more, faster.
Medical Coding
Our coding software offers a comprehensive suite of tools to make medical coding simple and intuitive for solo to large group practices.
Medical Scheduling
Our billing software is integrated with our scheduling and front office tools so you can collect payments with one-click display of patient information, copays and eligibility.
Payment Processing
Our billing software is integrated with our scheduling and front office tools so you can collect payments with one-click display of patient information, copays and eligibility.
Centralized Billing
Centralized medical billing with powerhouse performance. You can manage billing for each provider and location within a single database and login.
Cloud Hosted Medical Billing
More freedom, less equipment. Cloud-hosted medical billing keeps your data secure & saves you a bundle on equipment and IT costs.
ClaimInspector
ClaimInspector automatically scrubs your claims for CCI, HIPAA and LCD errors so you see an almost-100% first-pass claim acceptance rate.
Data Conversion Services
Let our data experts handle the data migration from your previous system.
eEligibility
Batch check patient insurance eligibility before appointments or perform on-demand checks with a simple click.
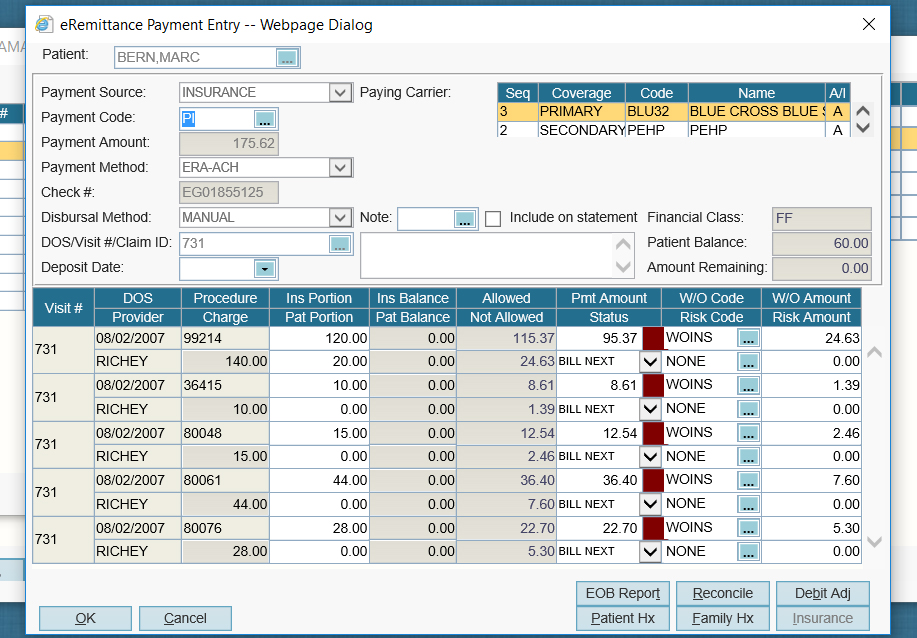
eRemittance
The automated ERA (electronic remittance advice) processing solution for independent practices.
EHR integration
Claims data and copay charges automatically pass into your electronic health records, so you don’t have to worry about manual processes and double data entry.
Why is AdvancedMD billing software highly rated?
Centralized, efficient claims management & billing
AdvancedMD, one of the world’s leading medical billing software companies, gives you all the tools you need to manage your claims process in one place and to ensure that your claims management and patient billing process run smoothly every time. Our robust clearinghouse automates manual processes and improves workflow with auto-generated worklists and claims status tracking for multiple providers and sites.
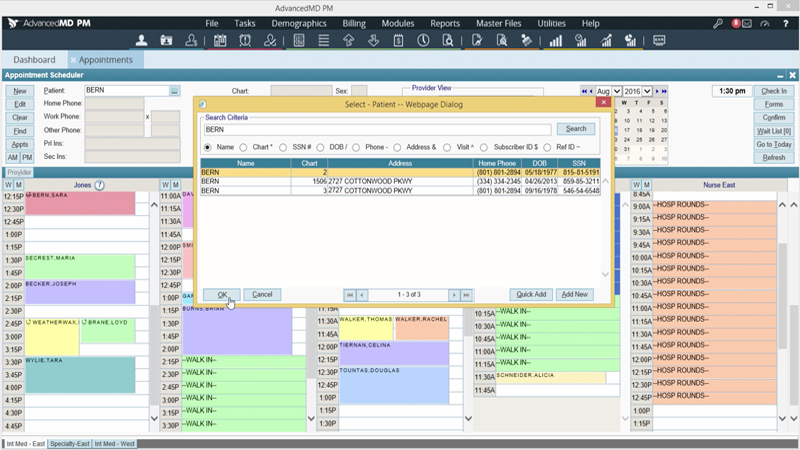
Smart scheduling can maximize your clinical efficiency.
Ensure your schedule stays full so your practice can accommodate more patients. Our powerful scheduling tools let you proactively manage no-shows, cancellations, waitlists and overbooking to maximize your clinical efficiency. Create recurring appointments and reminders to keep your patients and your practice on track.
Meaningful data to measure your financial performance.
Make informed financial decisions based on accurate, real-time data and gain a 360-degree view of your practice’s financial health. Our easy-to-read dashboard of interactive tools displays daily updates with MTD, YTD and period comparisons. Take advantage of big data technology, analytics and business intelligence to uncover your hidden revenue opportunities.
Frequently Asked Questions
Unable to find an answer you’re looking for? No problem. Chat with a live person and we’ll work to get your question answered.
What core workflows are covered by AdvancedMD medical billing software beyond basic claim submission?
The AdvancedMD medical billing suite manages the full claims lifecycle — including charge capture, eligibility verification (eEligibility), claims management, electronic remittance advice (ERA), patient payment processing, and collections — all from one centralized platform designed to reduce manual steps and improve reimbursements.
How does the A/R Control Center help practices improve collections?
The A/R Control Center provides dashboards with organized worklists, denial tracking tools, and actionable insights so staff can quickly identify problems, prioritize follow-up, and reduce days in accounts receivable — helping accelerate cash flow.
What is the Central Billing Office (CBO) feature and when is it useful?
CBO lets multi-provider or multi-location practices manage billing for all providers in a single database with one login, centralizing receivables, monitoring outstanding claims across locations, and improving coordination and visibility for billing teams.
How does AdvancedMD simplify claims scrubbing before submission?
ClaimInspector (often referenced as part of the billing software) automatically checks claims against coding and compliance rules (CCI, HIPAA, LCD) to help prevent errors that lead to denials, improving first-pass acceptance.
Does AdvancedMD offer insurance eligibility verification and what does it do?
Yes — eEligibility features let staff check patient insurance coverage in batches or on demand before visits, ensuring accurate billing and reducing surprises at check-in.
What kind of reporting and analytics does the billing software include?
The billing suite includes customizable financial reporting and analytics tools that help practices measure performance, track revenue trends, monitor payer data, and make informed decisions to improve financial outcomes.
Is the billing software cloud-hosted, and what does that mean for my practice?
Yes — the medical billing software is cloud-hosted, meaning data is stored securely offsite, accessible from any internet-connected device, and practices don’t need on-site servers or IT overhead for billing operations.
How does the integrated clearinghouse in AdvancedMD benefit billing teams?
The integrated clearinghouse automates claim submissions and remittance processing (ERA), eliminating the need to upload/download files manually and improving workflow efficiency.
Can AdvancedMD help with patient payments and point-of-care collections?
Yes — the billing suite integrates credit card processing and online patient payment tools so practices can collect copays and balances at check-in or through patient portals.
Does AdvancedMD offer data migration or conversion services for practices switching from another billing system?
Beyond software, AdvancedMD supplies training, documentation, and access to a partner ecosystem of more than 800 experienced RCM firms to assist practices directly.
What is the difference between in-house billing and outsourced RCM services with AdvancedMD?
Beyond software, AdvancedMD supplies training, documentation, and access to a partner ecosystem of more than 800 experienced RCM firms to assist practices directly.
Does AdvancedMD support billing companies or third-party medical billing services?
Yes — AdvancedMD has dedicated solutions for medical billing services, including centralized billing, customizable dashboards, and reporting optimized for billing companies managing multiple clients.
How does the software assist with denial management?
The system tracks denied claims and integrates denial workflows with A/R worklists so billing teams can quickly find root causes and resubmit clean claims — reducing lost revenue from outstanding denials.
How does AdvancedMD connect billing with clinical workflows?
Because AdvancedMD integrates billing with its practice management and EHR, charge data flows automatically from scheduling and clinical documentation into billing — reducing duplicate entry and mismatches between clinical records and claims.
What support and resources are available if my practice needs help with billing operations?
AdvancedMD offers professional services including implementation support, training, consulting, and connections to a network of more than 800 independent RCM partners — helping practices optimize billing workflows and outcomes.
Request a Live Demo
Complete the form below for a live demo to see all that AdvancedMD has to offer.