Get all the tools you need to manage your claims process in one place and to ensure that your claims and patient billing process run smoothly every time. Ensure your schedule stays full so your practice can accommodate more patients. Our powerful scheduling tools let you proactively manage no-shows, cancellations, waitlists, and overbooking to maximize your clinical efficiency.
The best medical billing & practice management software
Practice management software. Modern front office features.

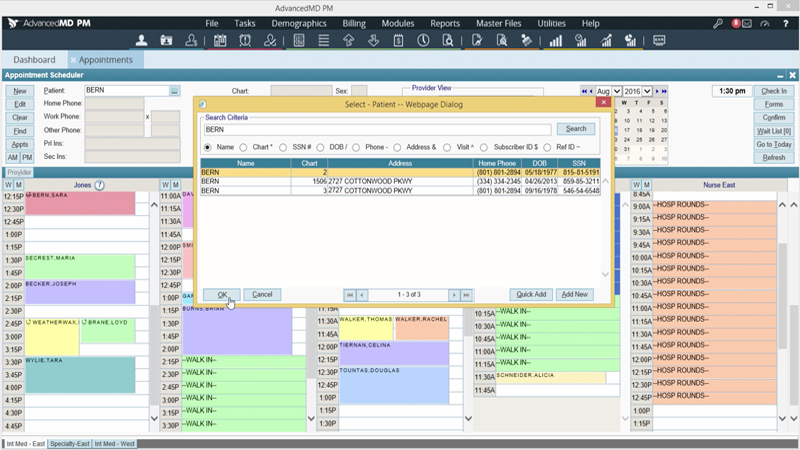
Scheduling Software
Quick-view and one-click features help your front office staff work faster and avoid time-consuming tasks like data comparisons.

Credit Card Processing
Minimize outstanding balances with built-in credit card processing and charge posting tools help you get paid faster and easier.

Check-in Kiosk
Take the hassle out of the check-in process. Collect insurance verification and copay forms quickly and easily from an iPad at your office
Insurance Verification
Automatically verifies insurance coverage for each patient prior to the appointment and updates patient files with the latest information.
Copay Collection
Integrated credit card processing help your staff quickly collect balances and post payments to patient accounts during check-in.
Charge Entry
Use our online charge slips to post procedure, diagnosis or modifier codes and set alerts for codes that require follow-up care.
Reporting Software
Measure your success and maximize your revenue with our exclusive, easy-to-use analytics and reporting tools.

Revenue Cycle Management
Outsource your medical billing processes and gain the insight to increase your practice revenue.
Time-Saving Support
Squeezed for time? We handle your unpaid claims, appeal secondary filings, exclusions and denials so you can focus on patients and practice growth
Comprehensive Care
Offload labor-intensive tasks including filing claims, working unpaid claims, exclusions, denials, filing appeals, secondary claim filing, payment posting and patient billing.
Boost your medical billing business.
Razor-sharp reporting, EHR integration and sales support help you run a more successful billing company.
Centralized Billing
Centralized medical billing with powerhouse performance. You can manage each provider, practice and location within a single database, with a single login.
Reporting & Analytics
Our reporting software provides you with timely, meaningful financial analytics and customized medical billing reports that help you maximize financial performance.

Frequently Asked Questions
Unable to find an answer you’re looking for? No problem. Chat with a live person and we’ll work to get your question answered.
What is the difference between AdvancedMD medical billing software and its full RCM services?
Our AdvancedMD billing software lets your practice manage claims, denials, and payments in-house using tools like eligibility, claims scrubbing, and dashboards, while our AdvancedMD RCM services let practices outsource the revenue cycle entirely, so an expert team manages claims, denials, posting, and collections on their behalf.
How does AdvancedMD help practices reduce denials before claims are submitted?
AdvancedMD includes an electronic claims scrubbing engine (often referenced in RCM content) that checks claims against compliance, code edits, and payer rules before submission to help maximize first-pass acceptance.
How does the AdvancedMD clearinghouse integration improve billing efficiency?
The built-in clearinghouse automates claim transmission and eremittance (ERA) rather than requiring manual uploads, enabling cleaner workflows and faster payment posting.
What tools are available to help practices track and manage A/R?
The AdvancedMD billing suite includes dashboards and worklists that let staff see outstanding claims, aging, denials, and follow-up tasks, helping reduce days in accounts receivable and prioritize high-impact work.
Can AdvancedMD help practices collect patient payments at the point of care?
Yes — with integrated credit card processing and patient payment tools, practices can collect copays and balances at check-in or bill patients online via statements.
What is the Central Billing Office (CBO) feature, and who benefits from it?
Central Billing Office features allow multi-location or multi-provider practices to manage all billing under one system with integrated dashboards and reporting, giving visibility across sites from a single login.
How does AdvancedMD support denial management workflows?
The system tracks denied claims and integrates them into A/R worklists so staff can follow up, correct issues, and resubmit claims — reducing lost revenue from untreated denials.
What reporting and analytics are included with AdvancedMD billing?
AdvancedMD offers robust reporting tools — including customizable financial and operational reports — to monitor revenue, payer performance, denials, and reimbursement trends.
How does the billing software connect with clinical and scheduling modules?
Because AdvancedMD billing is part of the unified cloud platform, charge information flows automatically from scheduling and clinical documentation into billing — reducing errors and duplicate data entry.
What support resources does AdvancedMD offer for billing teams?
Beyond software, AdvancedMD supplies training, documentation, and access to a partner ecosystem of more than 800 experienced RCM firms to assist practices directly.
Request a Live Demo
Complete the form below to sign up for a live demo of all AdvancedMD Billing features.