Implementing effective medical billing workflows not only helps streamline daily operations, but is key to building a thriving practice.
Your practice’s success relies on your ability to implement effective medical billing processes that not only drive efficiencies, but make it easier to receive payments from payors and patients. As a leading provider of medical billing solutions for private practices, AdvancedMD is laser-focused on building medical billing tools that help you meet your most critical medical billing needs.
But being a top provider of medical billing software means that we go beyond simply building technology that enables improved workflows across your practice—we prioritize keeping an ear to the ground when it comes to our customers’ biggest challenges. One of the ways we do this is by conducting customer surveys throughout the year so we know what’s impacting our community of ambulatory care providers, from their biggest challenges to their biggest wins.
Most recently, we polled our customers on their medical billing workflows, from payor processes and patient payments to staff sizes and whether or not they have a certified coder on staff. We’ve listed the full survey results below, but here are the primary takeaways:
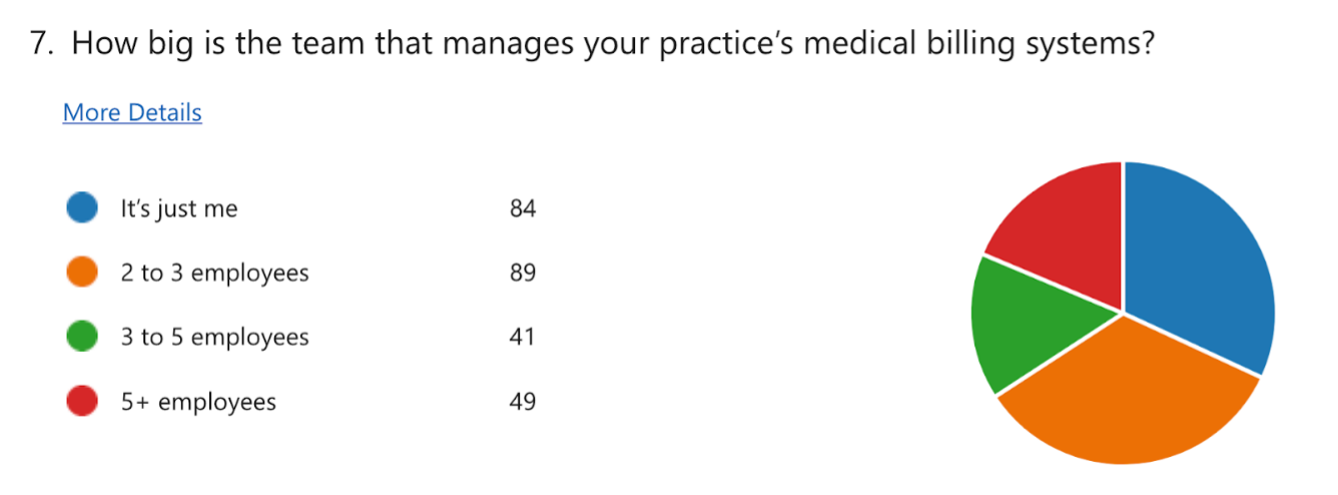
- More than 65% of the practices we surveyed have three or fewer employees managing medical billing processes—less than 20% have five employees or more handling medical billing.
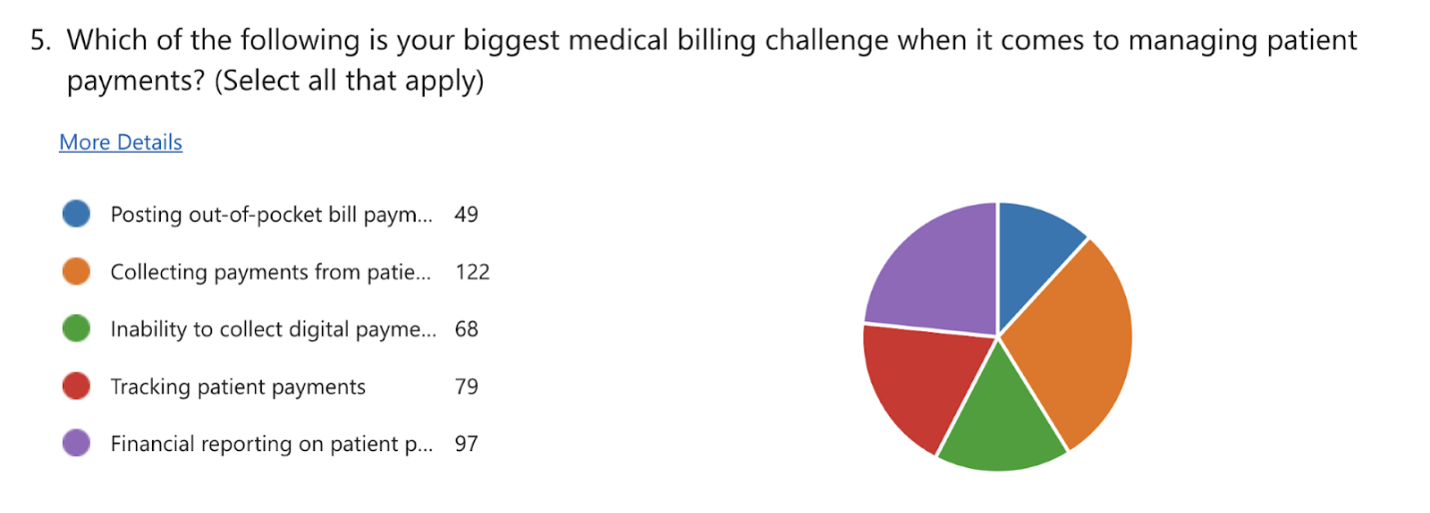
- Collecting payments from patients is the biggest challenge when it comes to patient payment issues. The biggest payor challenge: appealing denied claims.
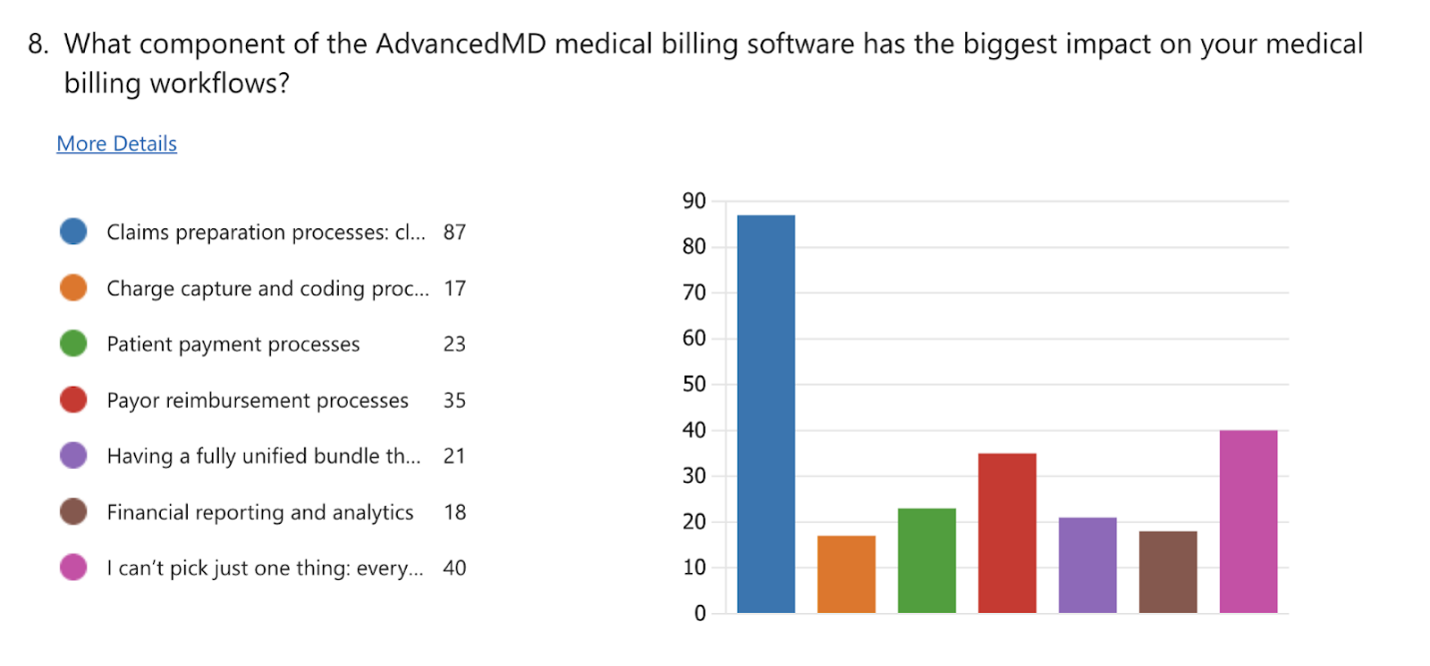
- According to our customers, the claims preparation component of the AdvancedMD platform has the biggest impact on their medical billing workflows.
AdvancedMD Customer Survey Findings:
1. When asked about managing commercial payor processes, 40% of survey respondents agreed or strongly agreed that they felt empowered to succeed.

2. Thirty percent of survey respondents agreed or strongly agreed that collecting patient payments is “easier than ever,” while 35% disagreed or strongly disagreed.
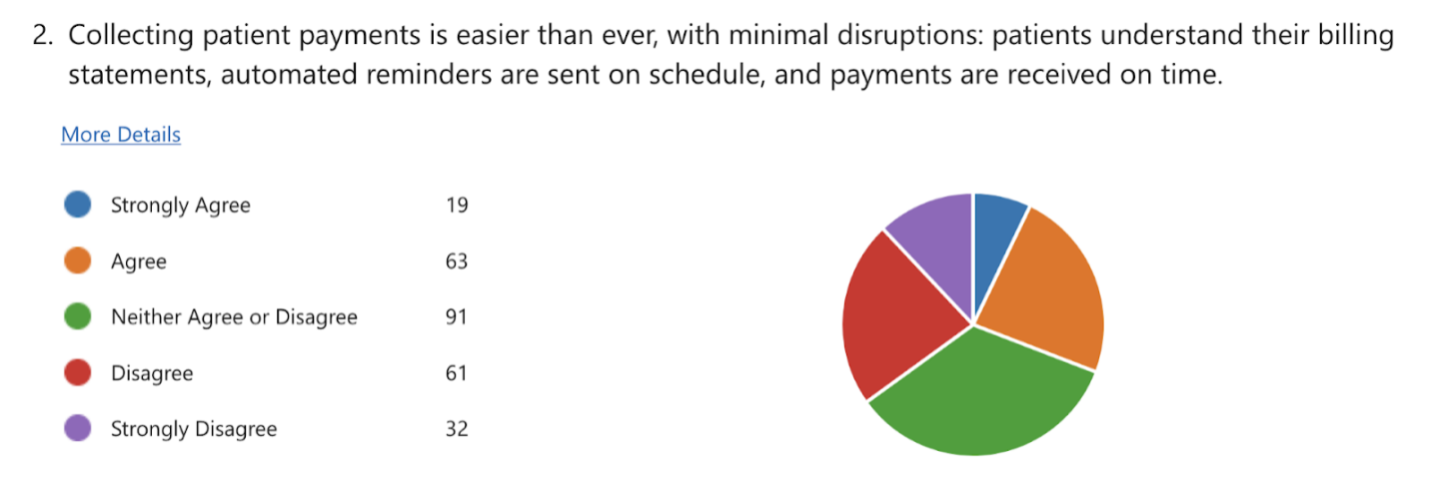
It’s worth noting that these results are likely impacted by medical debt more than the technology used to enable patient payments. According to the Consumer Financial Protection Bureau, 15 million Americans have medical bills on their credit report. A 2023 Healthcare Affordability Survey of more than 6,000 U.S. adults revealed more than 50% of respondents said it was somewhat difficult or very difficult to afford healthcare costs.
3. Survey respondents were nearly equally split when asked if their practice has all the tools it needs to implement and manage a successful revenue management strategy that ensures financial stability for their practice

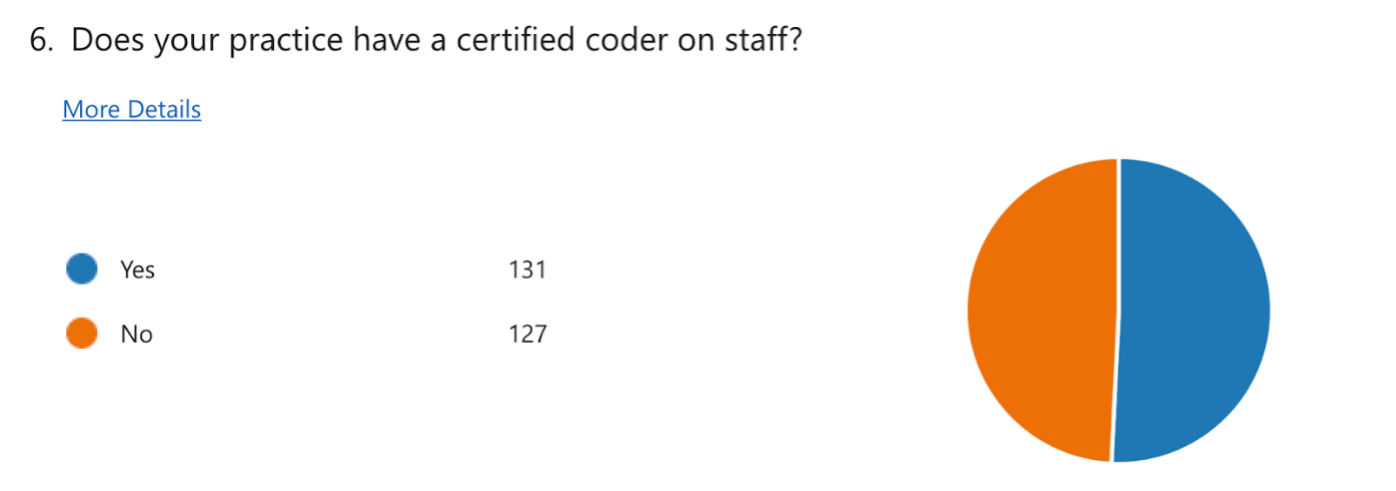
4. More than half of the survey respondents confirmed that their practice has a certified coder on staff.
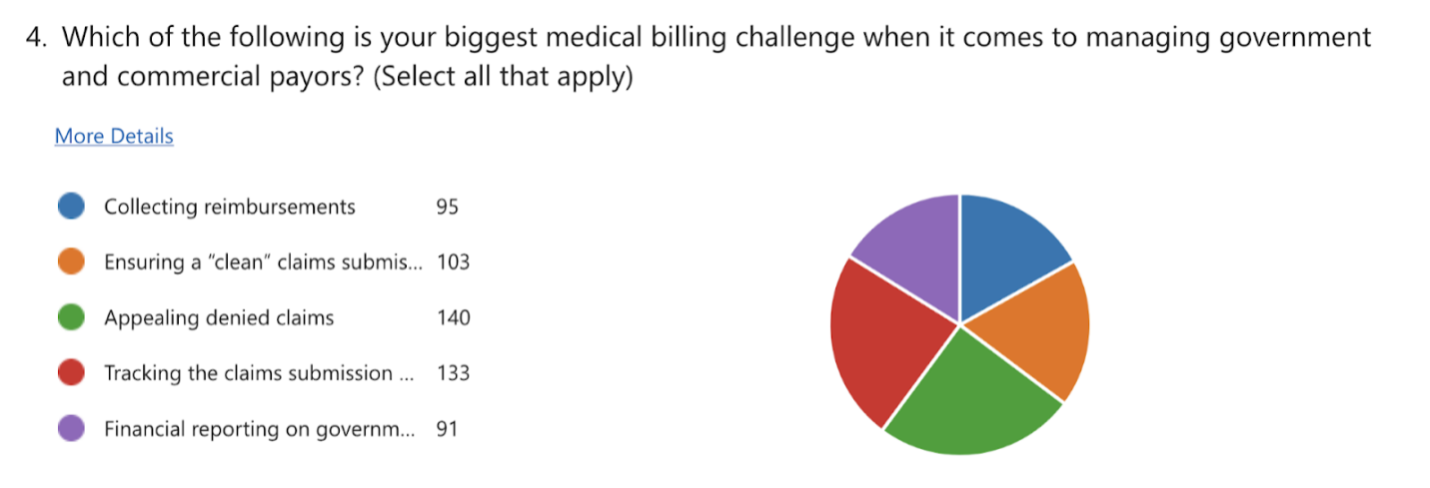
5. When asked about the biggest medical billing challenges associated with patient payments, the most cited response was collecting payments from patients.
6. More than half of the survey respondents confirmed that their practice has a certified coder on staff.
7. Sixty-five percent of survey respondents have three or fewer employees managing the practice’s medical billing systems.
8. When asked which component of the AdvancedMD medical billing platform has the biggest impact on the practice’s medical billing workflows, “claims preparation processes” was the most cited response by a wide margin.
The AdvancedMD customer survey was conducted online in June 2024 and included 266 responses

