Electronic health records (EHR) have become an essential part of every medical practice, with a significant number of clinics in the U.S. using these technologies. Despite widespread adoption, though, there are a lot of clinics that are unhappy with their current EHR. A 2016 report by Medical Economics found that more than half of EHR users (60%) either dislike their system or are neutral about it. However, the same report found that only 15% were considering switching EHR systems because they didn’t want to go through the hassle of implementing a new one.
That sentiment is understandable. EHR implementation, when not done right, can be costly. It can disrupt workflows, and it’s time-consuming. However, continuing to use an EHR that is not meeting your needs, is frustrating your physicians and staff, or is cumbersome to use can also be costly and time-consuming.
Rather than resigning yourself to using the wrong EHR, this two-part blog will provide the key steps in an implementation checklist to reduce the time and disruption to your clinic when you get a new (and much better) EHR system.
Step 1: Create a Full Implementation Plan
One of the places where many clinics fall short is in the planning stages prior to implementation. Once you have completed your evaluation of which EHR software is right for your practice, take some time to create a full and detailed plan of how you will implement—a roadmap, matrix, checklist, whatever you want to call it. This should include specific timelines for each step (you can get these from your EHR software vendor), and the team members who will be involved. Create a written version using free tools like Google Sheets, Asana, or Trello or find a subscription-based project management platform if necessary.
Step 2: Create a Committee and Designate a Champion or Lead
Depending on the size of your practice, you may want to create a separate committee that will take charge of the EHR implementation. Include a diverse representation of employees—physician(s), office manager, IT staff, medical billing, and clinical staff. If you have a relatively small practice, you may just put everyone on the committee. Regardless of practice and committee size, designate one person to be the “lead” or the “champion” for the project. They will communicate regularly with your software vendor and keep the project on track.
Step 3: Create a Budget
Before you start your EHR implementation it’s important to have a basic budget outline for the total costs. This includes any hardware or network upgrades, staff training (including overtime), and lost productivity. You can reduce some of these costs by choosing a cloud-based EHR so you won’t need servers or hardware. Also ask your vendor about any added costs, such as:
- Software customization
- Vendor training fees
- Consulting costs
- Data backup, storage, or transfer
It’s best if you can compare these costs before you sign a contract to avoid surprise fees and added costs during implementation.
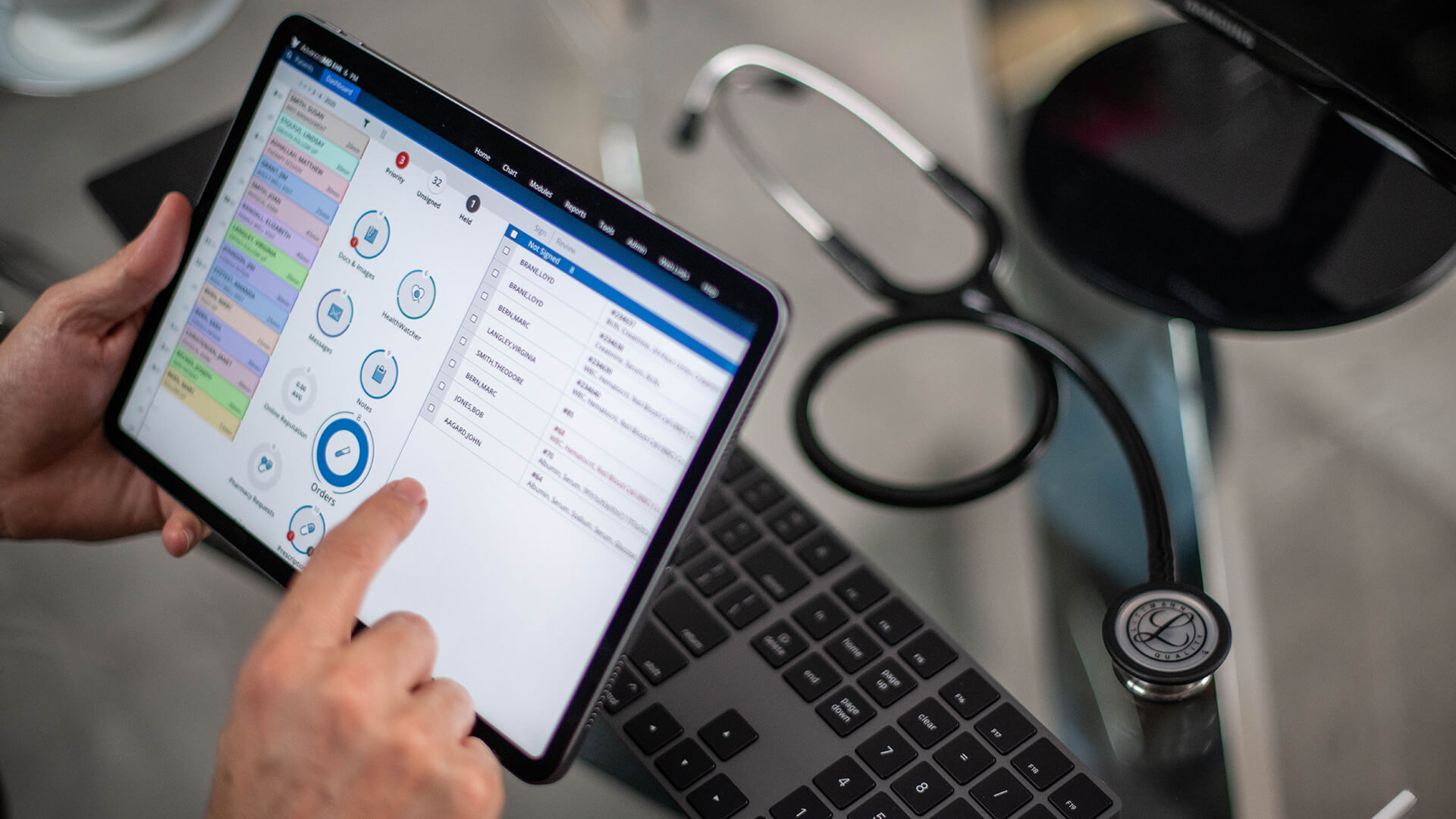
Check out AdvancedMD to see our intuitive and streamlined EHR solutions that easily integrate with your practice management software. Contact us today for a demo.

